2021 Study: Adipose Therapy for Ankle Osteoarthritis (2-Year Results)
Date: 30 January 2026
Admin: Medical Affairs
Every Step is a Decision
When you have ankle osteoarthritis, you don’t just walk—you negotiate. You scan the ground for uneven pavement. You dread the first few steps out of bed in the morning when the joint feels like a rusted hinge. You might even give up hiking or golf because the swelling afterward simply isn’t worth it.
If you’ve been living with chronic ankle pain after an old sprain, fracture, or sports injury, you know how much it can shrink your world. Walking on uneven ground, playing golf or tennis, even standing at a social event can go from automatic to exhausting.
For many people with ankle osteoarthritis (OA), the usual non-surgical options—bracing, anti-inflammatories, physiotherapy, cortisone or hyaluronic acid (“gel”) injections—only go so far. At the same time, ankle fusion or replacement are far less appealing, especially if you’re still active and relatively young.
- Ankle Fusion (Arthrodesis): This involves permanently locking the bones together with screws. It eliminates pain, but it also eliminates motion. You walk with a permanent alteration to your gait, and the stress is often transferred to other joints.
- Ankle Replacement: While technology is improving, these implants historically have higher failure rates and shorter lifespans than knee or hip replacements.
This creates a terrifying “waiting game.” You aren’t ready to fuse your ankle and lose your mobility, but the pain is becoming unmanageable.
A 2021 prospective study published in International Orthopaedics examined a compelling alternative. It followed patients with early-to-moderate ankle osteoarthritis for two full years after a single injection of their own micro-fragmented adipose (fat) tissue. The results suggest that this biologic approach can provide durable relief, potentially keeping you walking on your own natural joint for years longer.
This research examined micro-fragmented adipose tissue (MFAT), a treatment that shares foundational similarities with Regenerative Matrix Therapy™, RMIC’s next-generation biologic treatment. Our protocol was reviewed by Health Canada with no objection, offering a regulated, physician-led pathway for patients seeking to avoid the permanence of fusion.
The “Ankle Gap”: Why Conventional Care Fails
Unlike hip or knee OA, ankle OA is usually post-traumatic, often triggered by: old sports injuries, recurrent ankle sprains, malleolar fractures, ligament injuries, or joint deformities. As a result, patients are often younger and more active than typical hip or knee arthritis patients.
Standard treatments often fall short here:
- Cortisone: Can be helpful for acute flares, but cortisone weakens the already thin cartilage and other protective tissues of the ankle.
- Viscosupplementation (Gel): Often less effective in the ankle due to the tight joint space and complex mechanics.
- Surgery: As noted, the leap from “conservative care” to “surgery” is massive. There is no small fix for a worn-out ankle.
This leaves patients in a “treatment gap,” managing chronic pain while trying to preserve their lifestyle. The 2021 Natali study sought to bridge this gap by using the patient’s own biology to soothe the joint environment.
Learn More About Regenerative Matrix Therapy™
Study Overview: Two Years of Durability
- Study Design: Prospective clinical study following patients for 24 months.
- Population: 31 symptomatic patients (aged 28–71) with Early to Moderate Ankle Osteoarthritis (Takakura grades 2–3a).
- The Problem: All patients had chronic pain and functional limitation resistant to standard conservative management.
- Technique: Patients received a single intra-articular injection of autologous micro-fragmented adipose tissue (MFAT).
- Primary Goal: To evaluate safety and efficacy over a mid-to-long term (2 years).
- Endpoints:
AOFAS ankle–hindfoot score (0–100, higher = better function)
FADI (Foot and Ankle Disability Index, 0–100, higher = better)
Pain on a 0–10 VAS (higher = more pain)
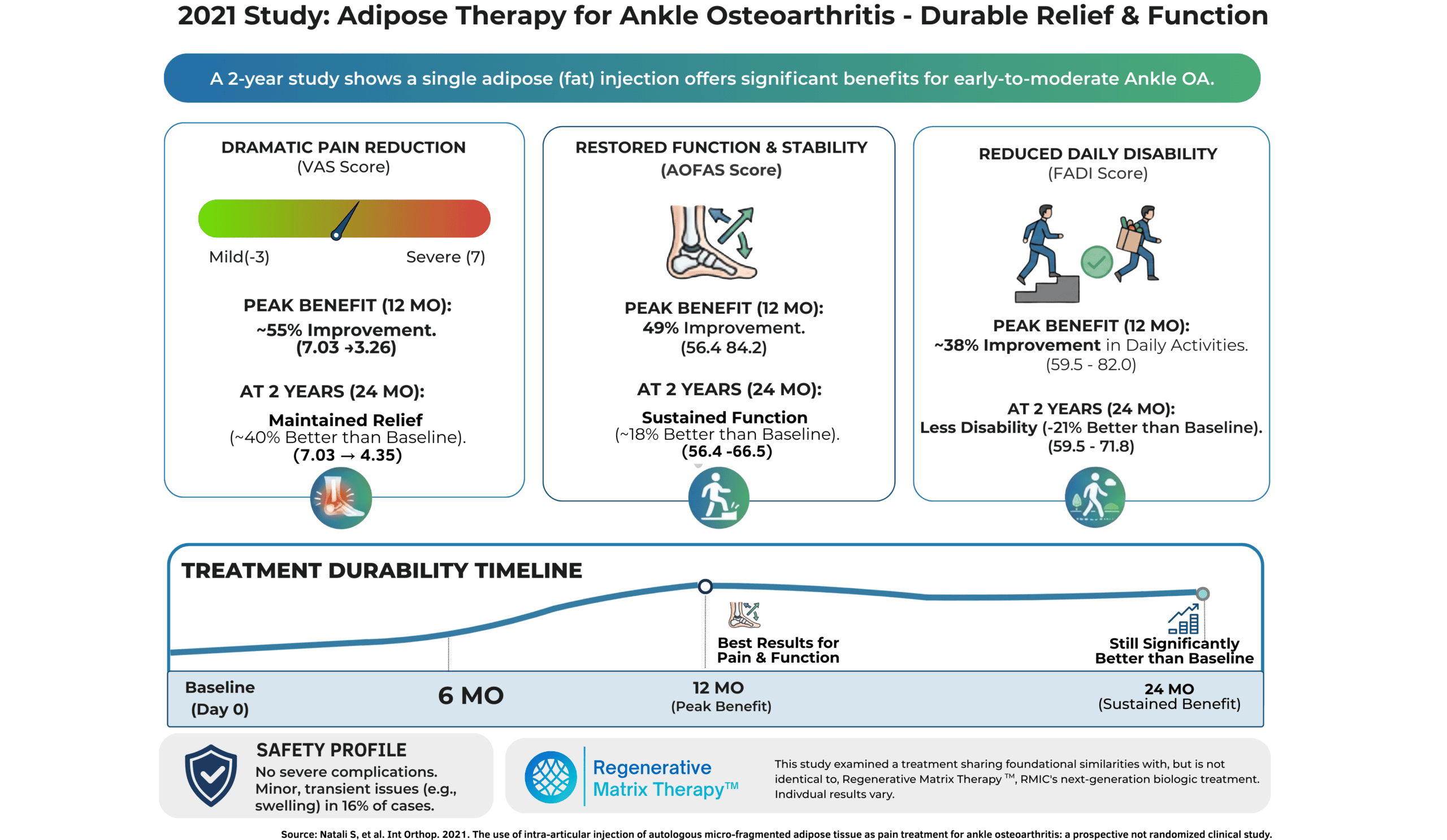
Key Findings: Durable Relief Without Implants
The standout finding of this study is not just that patients improved, but that the improvement held steady for two years. In many injection studies (like cortisone), results fade after a few months. Here, the biology provided a lasting effect.
- Dramatic Pain Reduction
Patients experienced a significant reduction in pain that was maintained through the 24-month checkpoint. Pain improved significantly at 6 months, continued to improve to the peak effect at 12 months and maintained benefit out to 24 months.
- The Stat: Pain (VAS) improved by ~50% at 6 months (VAS 7.03 → 3.61; p<0.005), continued to progress to peak effect with a ~55% improvement at 12 months (VAS 7.03 → 3.26; p<0.005), and continued to be effective with ~40% improvement at 24 months (VAS 7.03 → 4.35; p < 0.005).
- The Reality: Going from a distracting and limiting “severe” 7/10 pain to a mild-moderate ~4/10 (mild nuisance) is often the difference between sitting on the sidelines and getting back in the game for a full 2 years.
- Restored Function and Alignment
The study used the AOFAS (American Orthopaedic Foot and Ankle Society) score, which measures pain, function, and alignment. Patients experienced a notable boost in their abilities over time.
- The Stat: Function (AOFAS) improved by ~45% at 6 months after treatment (56.4 → 81.0) and continued to improve to its peak of a ~49% gain at 12 months (56.4 → 84.2).
- Durability: While some of the progress faded during the second year, the benefits didn’t disappear entirely. At 24 months, the average AOFAS score was 66.5, which is still an 18% improvement compared to baseline.
- Reduced Disability
Using the Foot and Ankle Disability Index (FADI), researchers measured how the ankle condition affected daily life.
- The Stat: Disability scores showed considerable improvements in everyday mobility and activity after treatment, with FADI scores rising by 26% at 6 months (59.5 → 75.1) and reaching a peak 38% gain at 12 months (59.5 → 82.0).
- Although some of the benefits diminished after the first year, there was still a statistically significant 21% improvement in function at 24 months after treatment (59.5 → 71.8)
- Significance: Higher scores mean less disability. Patients reported significantly less difficulty with activities like standing, walking on uneven ground, and climbing stairs.
- Durability & “Shape” of Response
- Improvements in pain and function peaked around 12 months, with a modest decline by 24 months.
- Even at 24 months, pain and function scores remained significantly better than pre-treatment levels across all metrics (AOFAS, FADI, VAS; all p<0.005 vs baseline).
- Safety
- No Severe Complications: No infections or major adverse events were recorded.
- Minor Issues: A small percentage of patients experienced transient abdominal pain (from the harvesting site) or mild joint swelling that resolved on its own within a few days.
What This Means for You: Keeping Your Options Open
If you have been told your ankle is “wearing out” due to ankle osteoarthritis (OA) and that fusion is in your future, this study suggests you may have a powerful alternative to buy time and maintain quality of life. This study using a single injection of a patient’s own fat offers some key takeaways:
- Pain relief can be substantial and sustained.
On average, patients cut pain scores roughly in half over the first year, with many maintaining meaningful relief at two years. The drop in VAS pain scores from a “7” (severe, distracting pain) to a “3” (mild, manageable annoyance) is life-changing. For many, this is the difference between sitting on the sidelines and getting back on the golf course or ski hill. - Function and daily activities improved significantly.
AOFAS and FADI scores reflect walking, stairs, standing, and recreational activities. A ~40–50% bump at 12 months suggests patients were able to do more, with less pain—often despite having failed physio, medications, steroid, or hyaluronic acid injections. - Benefits tend to soften over time, not disappear overnight.
The pattern in this cohort suggests many patients enjoyed their best results in the first year, with some waning by year two—but still better than baseline. This is consistent with how we think about biologic treatments: not as permanent “fixes,” but as interventions that can meaningfully shift the trajectory for a period of time. - Safe and Effective
Throughout the two-year follow-up, this study reported no serious side effects or complications. This finding highlights the benefits of using your body’s own tissue: it eliminates the need for surgery, donor products, or implants, and carries a lower risk.
Regenerative Matrix Therapy™, RMIC’s next-generation biologic treatment, is designed for exactly this type of patient—someone active who wants to preserve their natural joints for as long as possible.
At RMIC, we see this kind of study as directionally supportive of Regenerative Matrix Therapy™ for appropriately selected patients with ankle OA. Regenerative Matrix Therapy™ shares foundational similarities with the adipose-based approach used here—using your own fat tissue in a minimally invasive, image-guided procedure—but it is not identical, and results can vary from person to person. Our treatment protocol was reviewed by Health Canada with no objection and utilizes Precision Adipose Modulation™ to maximize the impact of the injection.
If you are in that difficult “in-between” zone—suffering from ankle pain but not ready to lock the joint with a fusion—Regenerative Matrix Therapy™ could be the solution that keeps you moving on your own terms.
Start Your Virtual Consultation
Research Highlights (for clinicians)
- Study Design: Prospective, non-randomized clinical study (n = 31 patients) of a single intra-articular injection of autologous micro-fragmented adipose tissue (MFat™/Lipogems®) for early-to-moderate ankle OA. Follow-up at 6, 12, and 24 months.
- Population: KL 1–3; mean age ~51; 27/31 post-traumatic; all had failed conservative care including injections.
- Effect Sizes (24 months):
- Pain (VAS): ~49% (7.0 → 3.6), ~54% (7.0 → 3.3), ~38% (7.0 → 4.4) improvements at 6, 12, 24 months respectively; all p<0.005 vs baseline.
- Function (AOFAS): ~44% (56 → 81), ~49% (56 → 84), ~18% (56 → 67) improvements at 6, 12, 24 months; all p<0.005 vs baseline.
- Disablity (FADI): ~26% (59 → 75), ~38% (59 → 82), ~21% (59 → 72) improvements at 6, 12, 24 months; all p<0.005 vs baseline.
- Safety: No severe complications; minor transient self-resolving pain at harvest/injection sites in ~16% of cases.
- Limitations: Small sample size, no control group, potential for placebo effect, single-center design.
- Stats: Paired one-tailed Student’s t-tests were used for within-subject comparisons; p<0.05 considered significant, with many comparisons achieving p<0.005.
- Follow-Up & Missing Data: All 31 patients met “completed follow-up” criteria at 6, 12, and 24 months; no imputation strategy described.
- Citation
Natali S, Screpis D, Farinelli L, Iacono V, Vacca V, Gigante A, et al. The use of intra-articular injection of autologous micro-fragmented adipose tissue as pain treatment for ankle osteoarthritis: a prospective not randomized clinical study. Int Orthop. 2021;45(8):2239-2244. doi:10.1007/s00264-021-05093-3.
Learn More About Regenerative Matrix Therapy™See More Conditions We Treat
Disclaimer
Regenerative Matrix Therapy™ shares foundational similarities with, but is not identical to, the treatment studied in this article. Individual results vary. Educational content only; not a substitute for professional medical advice.
Why Choose Regenerative Matrix Therapy™ with RMIC?
Ankle osteoarthritis is complex, and “standard” injections often fail to provide lasting relief. You need a protocol that addresses the biological environment of the joint.
Regenerative Matrix Therapy™ is RMIC’s next-generation, biologic-first treatment that uses your own adipose tissue, processed with our proprietary Precision Adipose Modulation™ method, to target joint pain and degeneration in a minimally invasive way. Our patent-pending protocol has been reviewed by Health Canada with no objection, and is delivered through a growing network of physician-led clinics across Canada.
Every patient undergoes a thorough assessment to determine whether Regenerative Matrix Therapy™ is appropriate for their specific joint, severity level, and goals. If you’re exploring ways to stay mobile, delay surgery, and maintain your lifestyle, our team can help you understand your options.
Don’t let a stiff ankle dictate your lifestyle.