2020 Study: Adipose Injection Helped Mild-to-Moderate Shoulder OA
Date: 27 November 2025
Admin: Medical Affairs
Can You Still Trust Your Shoulder?
It starts as a hesitation. You pause before reaching for the top shelf in the kitchen. You shorten your backswing on the golf course, sacrificing the power you used to take for granted. You wake up at 3:00 AM because you rolled onto your “bad side,” and the dull ache has turned into a sharp reminder that your body is changing.
For millions of Canadians, this is the reality of shoulder osteoarthritis (OA). It is a progressive, unforgiving condition that slowly steals your range of motion and your confidence.
If you are an “optimizer” – someone who skis in the winter, plays pickleball in the summer, and intends to stay active well into your 80s – the traditional medical menu for shoulder pain can feel dishearteningly limited. On one side, you have corticosteroid injections, which effectively mask the pain but may actually accelerate the deterioration of your cartilage with repeated use. On the other side, you have total shoulder replacement, a major surgical intervention that involves amputating the joint surface and replacing it with metal and plastic.
But what if you aren’t ready for metal? What if you just want your own shoulder to work like it used to?
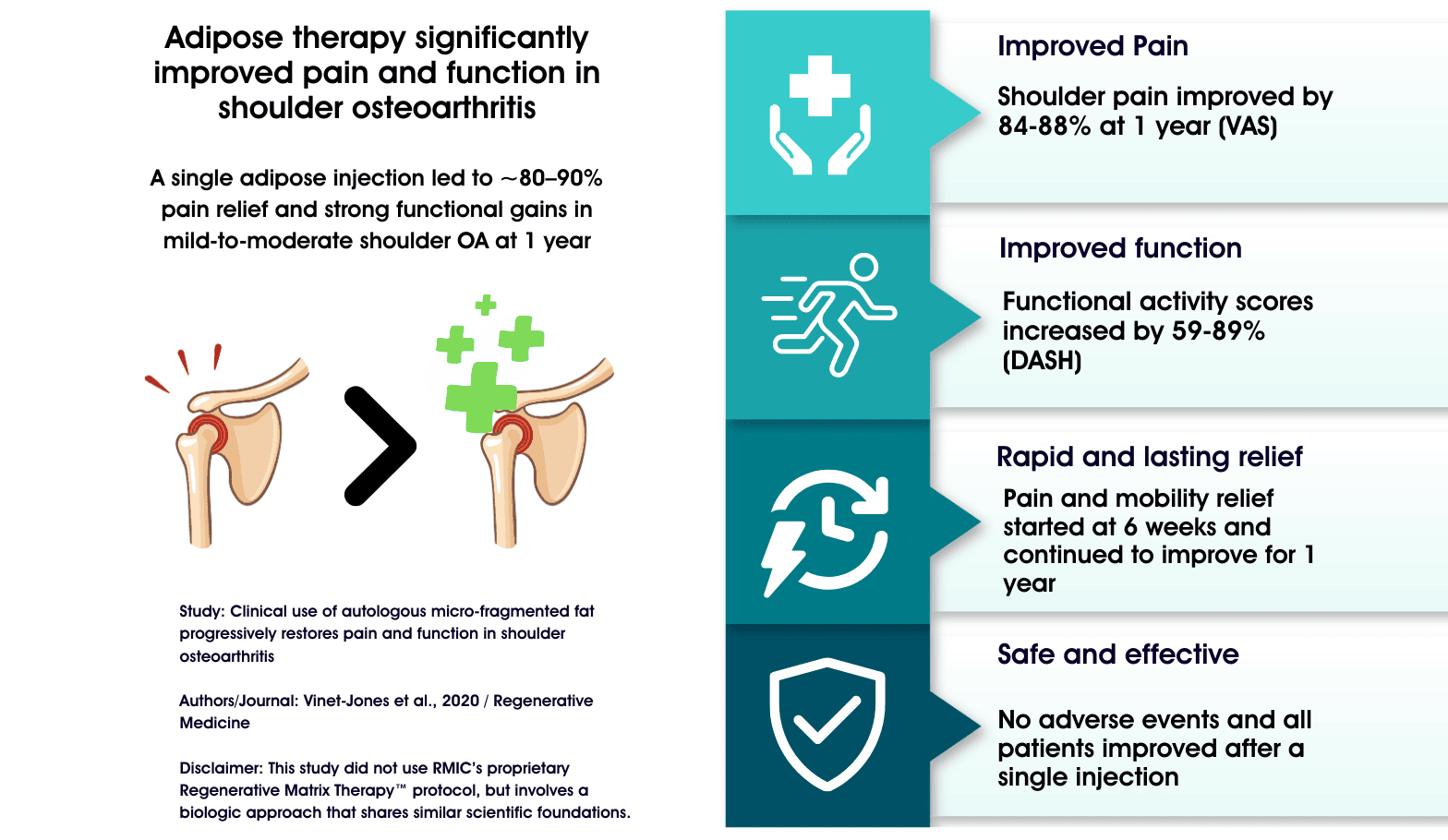
Adipose therapy for shoulder osteoarthritis is emerging as a potential non-surgical option in that frustrating middle ground. A pivotal 2020 study has illuminated this third path – adults with mild-to-moderate shoulder OA received a single ultrasound-guided injection prepared from their own fat (adipose tissue) and were followed for a year. Pain and function improved progressively over time, with average pain reductions in the ~80–90% range and strong gains in shoulder function. X-rays also showed increased joint space in the shoulder, an interesting but early structural signal.
This research examined micro-fragmented adipose tissue (MFat™), a treatment that shares foundational similarities with Regenerative Matrix Therapy™, RMIC’s next-generation biologic treatment. Our treatment protocol was reviewed by Health Canada with no objection and is delivered in a physician-led setting focused on safety and outcomes. The findings suggest that your body’s own fat tissue may hold the key to not just managing pain, but progressively restoring the function you thought was lost.
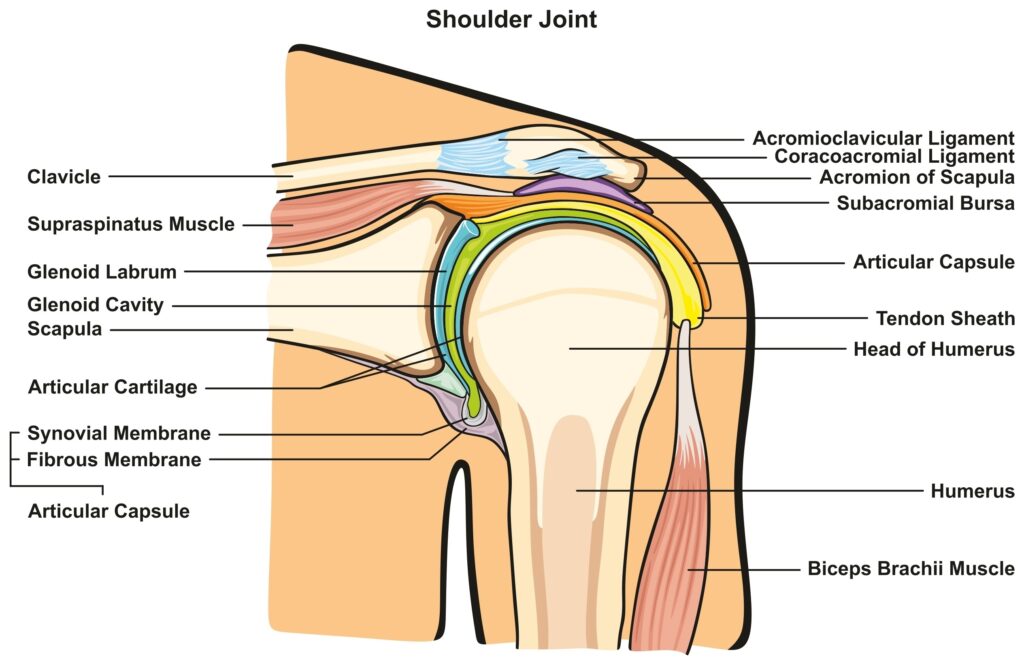
The Anatomy of the Problem: Why Shoulders Don’t Just “Bounce Back”
To understand why this research is so significant, we must first understand the “Shoulder Gap” in modern orthopedics.
The glenohumeral joint (the ball-and-socket joint of your shoulder) is a marvel of engineering, designed for an incredible range of motion.
However, this mobility comes at a cost. The articular cartilage and tissues that cushion the ball-and-socket joint have a notoriously poor blood supply. Unlike muscle or skin, which can regenerate after injury thanks to rich vascularization, cartilage has no built-in highway for delivering the nutrients and cells needed for repair. Once the cartilage and tissue starts to wear down, it stays down.
For years, the standard of care has been purely defensive: reduce inflammation (steroids) or replace the parts (surgery). There was no effective strategy to change the biological environment of the joint itself. Repeated steroid injections may even accelerate cartilage and tissue loss over time.
This is where the 2020 study by Vinet-Jones et al. changes the conversation. It explores using orthobiologic treatments as a “reparative” approach. Using the patient’s own biology to modify the disease environment – reduce pain and inflammation and potentially slow or even reverse the disease progression – rather than just suppressing its symptoms.
Study Overview: Turning the Tide on Degeneration
This prospective clinical study sought to determine if autologous micro-fragmented fat could serve as a viable, non-surgical alternative for patients trapped in the “Shoulder Gap.”
The study was rigorous in its design and patient selection, focusing on individuals who mirrored the exact demographic that often falls through the cracks: active adults with significant pain but a desire to avoid surgery.
- Study Design: Prospective, single-center clinical study on 25 patients (all over age 40) with confirmed symptomatic osteoarthritis of the glenohumeral joint.
- Severity Mix: The cohort included a mix of Mild (n=12) and Moderate (n=13) OA, classified by Kellgren-Lawrence (KL) grades 2 and 3.
- The Intervention: Patients received a single intra-articular injection of micro-fragmented adipose tissue (MFAT).
- Follow-Up: Patients were tracked for a full year (52 weeks), with data points at 6, 18, and 52 weeks to assess long-term durability.
- Primary outcomes:
- Pain: visual analog scale (VAS, 0–100).
- Function: Disabilities of the Arm, Shoulder and Hand (DASH) score.
- Exploratory outcome: X-ray measurement of glenohumeral joint space as a speculative correlate of cartilage status.
Key Findings: The “Progressive” Advantage
The most striking outcome of this study wasn’t just that patients got better – it was how they got better.
With traditional corticosteroid injections, patients typically experience a “cliff”: rapid pain relief that peaks within weeks and then wears off, often leaving the joint in worse condition than before. In contrast, the patients in this study experienced progressive improvement. The benefits didn’t fade; they compounded over time.
1. Rapid and Sustained Pain Reduction
Patients experienced a dramatic drop in pain scores (Visual Analog Scale – VAS) that began early and continued to improve or sustain throughout the year.
- Mild OA Group: Pain improved by ~52% at 6 weeks and had significant relief with ~88% pain improvement at 52 weeks / 1 year.
- Moderate OA Group: Pain improved by ~50% at 6 weeks and continued to improve to ~84% pain improvement at 52 weeks / 1 year, proving that even joints with more advanced wear can respond to biologic support.
2. Restoration of Function (The “Golf Swing” Metric)
Pain relief is important, but function is what allows you to live your life. The study used the DASH (Disabilities of the Arm, Shoulder and Hand) score to measure real-world capability and this also continued to improve throughout the year after treatment.
- Mild OA Group: Function improved by ~59% at 6 weeks and continued to improve to an ~89% function improvement at 52 weeks / 1 year.
- Moderate OA Group: Function improved by ~38% at 6 weeks and continued to improve to an ~59% function improvement at 52 weeks / 1 year.
- Significance: These numbers represent a transformation in daily life – the difference between struggling to dress yourself and returning to recreational sports.
3. Responder Rate and Joint Space on X-ray Increased
- Every single patient in this study reported significant improvements in pain and function, as early as 6 weeks after treatment.
- On repeat X-ray of the shoulder joint, there were statistically significant increases in the glenohumeral joint space, which the authors interpreted as a speculative sign of joint-structure modification
- Mild OA Group: ~22% increase in joint space at 6 weeks, and ~38% increase at 52 weeks / 1 year
- Moderate OA Group: ~22% increase in joint space at 6 weeks, and ~36% increase at 52 weeks / 1 year
4. Safety and Durability
- No Adverse Events: The procedure demonstrated an excellent safety profile, with no significant complications reported.
- One and Done: These results were achieved with a single treatment. There was no need for the repetitive, tissue-damaging series of injections often required with steroids.
What This Means for You: The Biological Difference
For someone with mild-to-moderate shoulder osteoarthritis, what do these numbers mean in day-to-day life?
- A ~80–90% average drop in pain at one year means many patients went from constant, activity-limiting pain to much milder, more manageable discomfort after a single adipose-based injection combined with a short course of supplements.
- Functional gains of ~60–90% on the DASH correspond to easier overhead reaching, improved sleep, and more confidence with work, sport, or simple tasks like putting on a jacket or carrying groceries.
- Improvements in the mild OA group kept building over the year, while the moderate OA group improved quickly and then held steady – suggesting that treating earlier in the disease process may offer more headroom for functional recovery.
Upon injection into the shoulder, the adipose (fat) may be able to:
- Reduce Inflammation: Switch off the chronic “fire” that eats away at your joint.
- Modulate pain and improve function: Allow your shoulder to move and function better.
- Provide Structural Support: Change the underlying disease process and potentially reverses some of its causes, including increasing the joint space on x-ray.
For patients considering advanced biologic options, this study is directionally supportive of the idea that a carefully delivered, fat-based treatment can offer durable, non-surgical relief for mild-to-moderate shoulder OA.
Regenerative Matrix Therapy™ is RMIC’s next-generation biologic procedure designed to reduce pain and inflammation while supporting joint health. Regenerative Matrix Therapy™ is delivered through a standardized, physician-led protocol that Health Canada reviewed with no objection. This study examined microfragmented adipose tissue, a related approach that shares foundational similarities with RMIC’s treatment. Regenerative Matrix Therapy™ is not identical to the intervention studied, but is a next-generation therapy based on some of the same principles. If you’re wondering whether a treatment like this could help delay or avoid shoulder surgery – or simply get you back to the activities you care about – the next step is a proper medical review of your case.
Start Your Virtual Consultation
Research Highlights
- Study Design: Prospective, single-arm, nonrandomized pilot study (n = 25 shoulders) of a single ultrasound-guided intra-articular injection of autologous micro-fragmented adipose tissue (Lipogems®) for mild-to-moderate glenohumeral OA. Follow-up at 6, 18, 52 weeks. Endpoints: VAS pain, DASH function, and exploratory GH joint space on radiographs. Stats: Kruskal–Wallis with Wilcoxon signed-rank post hoc; Mann–Whitney for KL 2 vs 3 DASH.
- Population and Severity: Adults >40 years with KL 2–3 glenohumeral OA (12 mild, 13 moderate); exclusions included BMI >45, significant cardiac disease, chronic immunosuppression, active smoking, and recent malignancy.
- Effect Sizes
- VAS pain (mild OA): ~52% → 77% → 88% improvement at 6, 18, 52 weeks.
- VAS pain (moderate OA): ~50% → 83% → 84% improvement at 6, 18, 52 weeks.
- DASH function (mild OA): ~59% → 77% → 89% improvement at 6, 18, 52 weeks.
- DASH function (moderate OA): ~38% → 63% → 59% improvement at 6, 18, 52 weeks.
- GH joint space: ~38% (≈ +1.13 mm) increase in mild and ~36% (≈ +0.9 mm) in moderate OA at 1 year (p < 0.05).
- Responder Signal: All 25 subjects showed significant improvement in pain and function at 6 weeks; mild OA continued to improve through 1 year, while moderate OA plateaued after 18 weeks, maintaining clinically meaningful gains.
- Safety: Outpatient lipoaspiration plus MFat™ injection with prophylactic antibiotics and standardized supplements; no serious adverse events were reported in the manuscript, though AE reporting was not detailed.
- Limitations: Single centre, small sample, no control or sham or active comparator, adjunct supplement regimen (cannot isolate injection effect), PRO-driven outcomes, imaging analysis limited to 18 shoulders with readable films, and potential placebo effect in patient-funded procedures.
- Citation:
Vinet-Jones H, Darr KF. Clinical use of autologous micro-fragmented fat progressively restores pain and function in shoulder osteoarthritis. Regener Med. 2020;15(10):2153–2161. doi:10.2217/rme-2020-0069.
Learn More About Regenerative Matrix Therapy™See More Conditions We Treat
Disclaimer
Regenerative Matrix Therapy™ shares foundational similarities with, but is not identical to, the treatment studied. Individual results vary. Educational content only; not a substitute for professional medical advice.
The RMIC Advantage: Why Protocol Matters
While the results of this study are groundbreaking, the success of regenerative medicine depends entirely on the quality of the protocol. Not all treatments are created equal.
The Regenerative Medicine Institute of Canada (RMIC) is the only organization in the country that has successfully navigated the scrutiny of federal regulators for this specific type of therapy.
- Our Regenerative Matrix Therapy™ protocol has been reviewed by Health Canada with no objection.
- Regenerative Matrix Therapy™ is a next-generation biologic treatment delivered under a standardized protocol delivered by qualified physicians
- We use our proprietary Precision Adipose Modulation™ to purify your adipose tissue and maximizing its ability to drive results
You don’t have to accept “bone-on-bone” as the end of your active life.
If you are ready to explore a treatment that targets the source of your pain rather than just masking it, we invite you to start the conversation.